Step 3: Verify the Diagnosis
Verifying the diagnosis, is closely linked to verifying the existence of an outbreak. In fact, often these two steps are addressed at the same time. Verifying the diagnosis is important: (a) to ensure that the disease has been properly identified, since control measures are often disease-specific; and (b) to rule out laboratory error as the basis for the increase in reported cases. (CDC, 2012, p. 425)
For this verification, it is necessary to get clinical information regarding the cases as well as their laboratory results, where tests had been requested. The information is used to evaluate predominant signs and symptoms, incubation period, duration of symptoms, laboratory testing, and transmission route.
Incubation Period
After the disease process has been triggered, pathological changes then occur without the individual being aware of them. This stage of subclinical disease, extending from the time of exposure to onset of disease symptoms, is usually called the incubation period for infectious diseases, and the latency period for chronic diseases. During this stage, disease is said to be asymptomatic (no symptoms) or inapparent.
For a newly recognized disease, field investigation provides an opportunity to characterize the natural history — including agent, mode of transmission, and incubation period — and the clinical spectrum of disease. Conversations with patients are very useful in generating hypotheses about disease etiology and spread.
Frequency distributions of the clinical features are useful in characterizing the spectrum of illness, verifying the diagnosis, and developing case definitions (CDC, 2012)
Some examples of such distributions are provided in the table below.
Clinical Features of the Main Types of Foodborne Illness

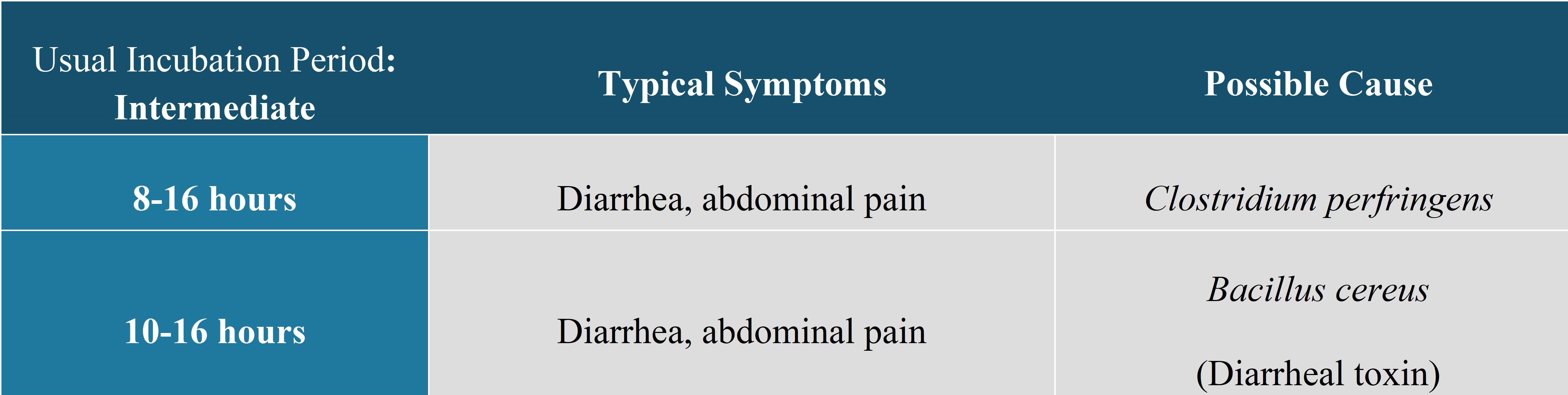

The signs and symptoms present can provide clues to the etiological agent. This information, coupled with that of the probable source or vehicle, the presumed mode of transmission and the probable incubation period, can help the investigator select the appropriate laboratory tests to perform.
It is essential to confirm a sufficient number of cases using laboratory analyses (when such tests exist). This must be done from the very beginning of the investigation. In fact, it is possible that relatively few cases occur after the initial reporting of the event. In cases of gastroenteritis, it is also preferable to take the specimens at the acute phase (e.g., within 72 hours from the onset of symptoms). Specimens taken late (e.g., during the convalescent phase or after the beginning of antibiotic treatment) may not identify the agent. For an outbreak with a large number of cases, it is usually sufficient to confirm 15% to 20% of them.
If the outbreak persists, it is necessary to conduct laboratory tests among a certain number of new cases to confirm that the agent is still circulating.
Frequently, the laboratory analyses related to the etiological agent are conducted routinely on all of the specimens that are submitted. The investigator does not then have to specifically request confirmatory testing for a proportion of submitted samples. Nevertheless, apart from the confirmation tests, characterization analyses (typing, sub-typing) of the isolates may be necessary. In these circumstances, specimens and isolates must be preserved and sent in a timely manner to the regional reference laboratory. These regional reference laboratories usually take the precaution of preserving a sample of the strains that may then be sent on to national or international laboratories for more specific tests, such as phage typing.
Working with the laboratory during outbreak investigations:
- flag samples with an "outbreak identifier"; this ensures the lab can report all positive and all negative results, and all results for more specific testing;
- consult the microbiologists or other specialists on the types of tests to be conducted as well as the modalities of specimen collection, conservation and transportation;
- ensure that the necessary tests are available and are conducted (some analyses are only made on special request);
- verify their ability to analyze an increased number of samples (e.g. sufficient human resources [laboratory technicians], available culture media, etc.);
- ask that the specimens and isolates be preserved for eventual sub-typing, when appropriate (usually, they are not routinely kept in front-line laboratories due to limited space and the associated costs).
References
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), Office of Workforce and Career Development. (2012). Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics (3rd ed.).
