Step 4: Construct a working case definition
A case definition is a set of uniform criteria (of inclusion and exclusion) used to decide whether an individual will be considered to have the disease of interest for the purpose of the investigation. Simple objective criteria are usually best.
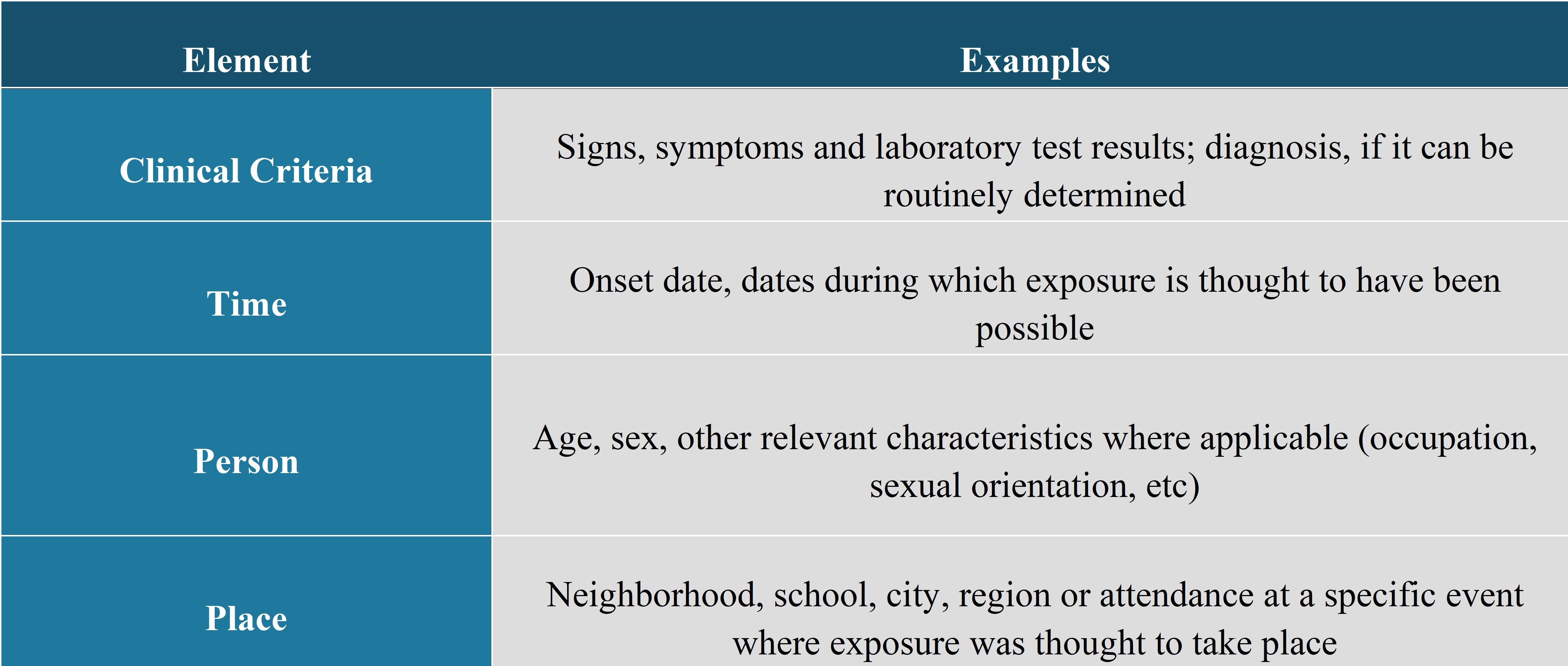
A good case definition will include the elements:
Elements of a Case Definition
The clinical syndrome refers to symptoms related to the clinical history and to signs observed during the physical examination. The symptoms are frequently more subjective whereas the clinical signs are frequently more objective.
Example:
Symptoms: e.g., headache, myalgia, vomiting, diarrhea, etc.
Clinical Signs: e.g., measured temperature of 38.5°C or more, hepatomegaly, maculopapular rash, etc.
It may be necessary to define certain terms, such as diarrhea (e.g., liquid or loose stools or one that takes on the shape of the container) and to specify the number of episodes required, and the degree of severity of the symptom, in order to consider an individual as being a case (e.g., 2 episodes of vomiting or 3 episodes of diarrhea within a 24-hour period, fatigue that interferes with normal daily activities, etc.). A combination of symptoms and clinical signs is frequently used in the case definition (e.g., the presence of at least three of the following symptoms or signs: fever, myalgia, periorbital edema, eosinophilia > 500 cells / mm 3).
Results of laboratory tests (e.g., presence of IgM antibodies or four-fold increase or more of IgG antibodies against an agent between the serum in an acute stage and the serum at convalescence, positive culture for an agent, specific profile of the agent [results of an antibiogram, phage-typing, pulsovar], etc.), when these analyses are available, or other examinations or tests (e.g., pneumonia or pleural effusion shown on a chest X-ray, other results of medical imagery, etc.), can be added to the definition of cases. This increases the degree of certainty regarding the disease, as different agents can cause similar clinical syndromes (e.g., viral hepatitis caused by hepatitis A, hepatitis B, hepatitis C, etc.). It could also be that the outbreak is due to a specific sub-type of an agent (e.g., S. enteritidis of a specific phage-type, L. monocytogenes of a specific pulsovar, etc.). The degree of confirmation required should be based on available testing. For example, it should not be required that all the cases undergo an invasive test (e.g., muscular biopsy in cases of trichinosis) when other types of valid analyses (such as serology) are available.
A case definition includes clinical criteria and - particularly in the setting of an outbreak investigation - restrictions by time, place, and person. (CDC, 2012)
Time: e.g., an illness that occurred between a range of dates or during the last X weeks, etc.Place: e.g., residents of province P or who had visited region R during a certain time period, patients or employees of a certain institution, etc.
Person: e.g. specific age group, individuals without antecedents of such an illness or with no history of vaccination against this disease, persons with a cochlear implant, members of a particular group, etc.
If the disease and its incubation period are known, the epi curve can be used to deduce a probable time of exposure and help develop a questionnaire focused on that time period (CDC, 2012).
Below is an example of a case definition during a point-source foodborne outbreak of Clostridium perfringens using the incubation period (note that, even if this definition was not very specific regarding abdominal cramps, all the cases had diarrhea during this event).
Case definition in a foodborne outbreak caused by Norovirus at a manufacturing company
"Person working in the affected unit with onset of diarrhoea and/or vomiting between 11:00 hours (13 November) and 13:30 hours (14 November)"
Zomer, et al., 2010
An epidemiological link to another case may be included in the definition for infections communicable from person to person. For example, an individual presenting a specific clinical presentation but who had not been confirmed by laboratory tests can be considered as a case if he had been in contact with a laboratory-confirmed case during the incubation period that is recognized for the illness of interest. This approach is regularly used for illnesses that are preventable by vaccination and for enteric diseases. Below is an example for measles.
Case Definition
Case definitions developed for surveillance can serve as inspiration in the creation of a case definition for an outbreak. However, they may require adaptation (e.g., the addition of a "probable" class, the distinction between primary and secondary cases, time frames etc.). The case definitions included in investigation reports of other similar outbreaks, whether published or not, can also serve as models. Solicit feedback from colleagues or consultants on a draft case definition to ensure that it meets the investigation needs and is feasible.
The classification of cases into possible (presumed or suspected), probable (clinical) and confirmed (definite or certain), as in the COVID-19 case below, allows us to "manage" the uncertainty of the diagnosis. Cases categorized as "confirmed" must generally (but not always) be confirmed through laboratory analyses. Those classified as "probable" generally have a clinical presentation that is typical of the illness of interest but without confirmation by laboratory analysis. Finally, those classified as "possible" have only some of the features of a "probable" case. Generally speaking it is wise to include symptoms and clinical signs in the "confirmed" class to distinguish symptomatic infections from asymptomatic colonization.
Case definition of infection with COVID-19
Confirmed case:
Probable case:
- A suspect case for whom testing for the COVID-19 virus is inconclusive.
- A suspect case for whom testing could not be performed for any reason.
Possible case:
- A patient with acute respiratory illness (fever and at least one sign/symptom of respiratory disease, e.g., cough, shortness of breath), AND a history of travel to or residence in a location reporting community transmission of COVID-19 disease during the 14 days prior to symptom onset.
- A patient with any acute respiratory illness AND having been in contact with a confirmed or probable COVID-19 case (see definition of contact) in the last 14 days prior to symptom onset.
- A patient with severe acute respiratory illness (fever and at least one sign/symptom of respiratory disease, e.g., cough, shortness of breath; AND requiring hospitalization) AND in the absence of an alternative diagnosis that fully explains the clinical presentation.
Case classification is useful from several perspectives. First, this allows follow-up of case files according to available information. A case may provisionally be classed as "possible" while awaiting information on the clinical presentation and the results of laboratory analyses. This casts a wide net for people who may be part of the outbreak. A certain proportion of the cases will never be confirmed due to the high cost of analyses, the difficulties of conducting the tests or because this confirmation is not judged to be necessary. Regardless, it is likely that they are part of the outbreak and that information from them will help to identify the cause.
Yet, at a certain phase in the investigation, it may be decided to reinforce the validity of the results and use only the information from confirmed cases. For example, the cases classified as "possible" in the case above, were excluded from the case-control study aimed at determining the food vehicles that were responsible for the outbreak. The inclusion of "false positive" cases during an analytical study can lead to errors in the interpretation of results.
During the investigation of an outbreak of a disease that is communicable from person to person, it is important to distinguish primary cases from secondary ones.
Primary Case
A case whose symptoms appeared following exposure to the presumed source (within the minimum and maximum limits of the known incubation period of the illness). When there is more than one primary case in given place, they are called "co-primary" cases.
Secondary Case
A case whose symptoms appeared after contact with a primary case (within the minimum and maximum limits of incubation) but without exposure to the presumed source.
Finally, remember that the case definition is a tool for classifying people into categories. How people are classified affects what is done with them or their information. Case definitions can change during an investigation, although this should not be done lightly as is tends to cause confusion. As the data is analysed, the inclusion criteria may be changed, in a logical way, to match the hypotheses.
References
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (CDC), Office of Workforce and Career Development. (2012). Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics (3rd ed.).
World Health Organization (WHO). Global surveillance for COVID-19 caused by human infection with COVID-19 virus: interim guidance. https://www.who.int/publications/i/item/global-surveillance-for-covid-19-caused-by-human-infection-with-covid-19-virus-interim-guidance
Zomer, T., DeJong, B., Kühlmann-Berenzon, S., Nyren, O., Svenungsson, B., Hedlund, K., Ancker, C., Wahl, T., & Andersson, Y. (2010). A foodborne norovirus outbreak at a manufacturing company. Epidemiology and Infection, 138(4), 501-506. https://www.jstor.org/stable/40603219
