-
GeneralGeneral
-
Depression Counseling Homepage
This Depression Counseling introductory course provides a fundation of theoretical and practical knowledge and skills to develop psychological treatments for patients with moderately severe to severe depression, which can be scaled up in routine health care settings. All parts of this training are free, including registration, learning, testing, and a certificate of completion. This course is intended for primary-care physicians, nurses, and allied health professionals in training and practice.
This Depression Counseling course is based on the Healthy Activity Program (HAP) manual, it was developed in partnership with the PREMIUM program funded by the Wellcome Trust, in association with the London School of Hygiene & Tropical Medicine, Sangath organization, and the Government of Goa's Directorate of Health Services. The course was developed by Arpita Anand, Sona Dimidjian, and Vikram Patel; additional contributions were made by Angela Leocata, Sydney Church, Luanna Fernandes, Ajay Kumar, Akila Kalsur, Ankita Khanna, Medha Upadhye, and Dielle Dsouza. The authors of the manual are Arpita Anand, Neerja Chowdhary, Sona Dimidjian, and Vikram Patel.
For a publication on this course’s efficacy, see “The Healthy Activity Program (HAP), A Lay Counsellor-Delivered Brief Psychological Treatment for Severe Depression, in Primary Care in India: A Randomised Controlled Trial,” (2017), The Lancet, https://doi.org/10.1016/S0140-6736(16)31589-6; see also “Building Public Health Capacity through Online Global Learning,” (2018), Open Praxis, to see more research related to NextGenU.org’s educational model, check out NextGenU.org’s publication page. Subscribe to our newsletter to be notified of future updates, new courses, and to be part of our community.
There are 12 modules which provide:
- An overview of important concepts in counseling for depression,
- Skills to identify patients with depression,
- Techniques of behavioral activation for treating depression,
- Strategies in dealing with problems that may be experienced by people with depression.
Approximate time for completion of this course is 9 hours at an average reading rate of 144 words/minute.
At the end of each lesson, there is a practice quiz. At the end of the course, after you’ve completed each lesson, quiz, and activity, you’ll have access to a final exam, and a chance to assess the training. Once you’ve passed that last test, you will be able to download a certificate of completion from NextGenU.org and our course’s co-sponsoring organizations (listed above). We keep all of your personal information confidential, never sell any of your information, and only use anonymized data for research purposes, and we are also happy to report your testing information and share your work with anyone (your school, employer, etc.) at your request. We hope that you will find this a rewarding learning experience, and we count on your feedback to help us improve this training for future students.
Engaging with this Course
You may browse this course for free to learn for your personal enrichment; there are no requirements.
To obtain a certificate
- Show in the registration fields that you have the appropriate prerequisites to be certified. This course requires the learner to have already obtained a college-level degree.
- Complete all the reading requirements.
- Complete all quizzes and pass with a 70% with unlimited attempts.
- Successfully complete the final exam with a minimum of 70% and a maximum of 3 attempts.
- Complete the self and course evaluation forms.
To obtain credit
- Complete all requirements listed above for the certificate.
- Your learning institution or workplace should approve the partner-university-sponsored NextGenU.org course for educational credit, as they would for their learner taking a course anywhere.
- NextGenU.org is happy to provide your institution with:
- a link to and description of the course training, so they can see all its components, including the cosponsoring universities and other professional organization cosponsors;
- your grade on the final exam;
- your work products (e.g. peer and mentored activities), and any other required or optional shared materials that you produce and authorize to share with them;
- your evaluations - course, and self-assessments;
- a copy of your certificate of completion, with the co-sponsoring universities and other organizations listed.
To obtain a degree co-sponsored with NextGenU.org, registrants must be enrolled in a degree program as a student of a NextGenU.org institutional partner. If you think that your institution might be interested in offering a degree with NextGenU.org contact us.
We hope that you will find this a rewarding learning experience, and we count on your assessment and feedback to help us improve this training for future students.
Next Steps
- Complete the registration form.
- Begin the course with Module 1: Depression - An Introduction. In each lesson, read the description, complete all required readings and any required activity, and take the corresponding quizzes.
This course meets nationally approved standards of education developed for the addiction/substance use disorders counseling profession. This course's participants are assured that the continuing education (CE) credits provided will be accepted toward national credentialing by the NAADAC Certification Commission for Addiction Professionals (NCC AP), as well as by many of the individual state licensing/certification bodies in the addiction and other helping professions.
-
Module 1 : Depression - An Introduction.
Kamala is a 50-year-old woman with three children. Her husband left her when her children were small, and she takes care of them by herself. Her eldest daughter has a well-paying job and her other two children are in school. Kamala was happy that her daughter could help to financially support the family, until she became involved with a married man of the locality. She now lives with him and no longer speaks with Kamala or her family. Since this time, Kamala has been very upset. She feels very hopeless, tired, and irritable, and she has been having difficulty sleeping and eating.
Manisha is 35 years old and lives with her husband and two children. Her husband hasn't had a regular job for several years, has a drinking problem, and often beats her. Manisha's two married sisters support her and her family financially. She recently took up a job, but is unable to focus on her work, feels tired, and sleeps poorly. She has lost interest in life and attempted suicide two months ago.
Harish is a 25-year-old driver who recently left his job in the city to come back to his village. His wife thought he was having affairs with other women in the city and wanted him to return. Harish does not have a job in the village, spends most of his time in the house, and often fights with his wife. He says that he feels irritable and tired most of the time, having lost interest in activities he used to enjoy, and has been having difficulty eating and sleeping.
Meena is 42 years old and says she feels tired, has body aches, difficulty sleeping, and is unable to focus on her work as a teacher. Her husband died in an accident three months ago and she misses him very much. She remembers the plans they had for the future and worries about how she will manage without him. She avoids family and friends, misses work often, and spends most of her time alone at home, crying or lying in bed for hours.
We may meet patients like Kamala, Manisha, Harish, or Meena in our work at the Primary Health Clinic (PHC). With what are they struggling, and how can we help them?
-
Module 1: Lesson 2: Symptoms
Watch the video lecture in the activities section below to learn about the symptoms of depression
There are three important features that you must keep in mind when noting down signs that a patient might have depression:
- How many and which symptoms are present
- When and how often they occur
- Their effect on the patient’s functioning
The number and length of the symptoms, and their effect on the patient’s functioning, show how depression is different from everyday sadness
Physical Feeling Thoughts Actions Tiredness Sadness Hopelessness Withdrawal from social interaction Weakness Irritability Difficulty in making decisions Inability to work or perform other responsibilities Aches and pains Losing interest in things Thinking of oneself as worthless Withdrawal from enjoyable activities Disturbed sleep Guilt Thoughts about dying or killing oneself Poor appetite 1 URL -
Module 1: Lesson 3: Detecting Depression
Watch the video lecture in the activities section below to learn how to know if your patient has depression
SUMMARY
- Depression is a stress-related illness that can be caused by many biological, psychological and social factors.
- Depression can show itself in different ways; in a PHC, patients are more likely to seek treatment for the physical symptoms linked to depression.
- Identifying if a patient has depression depends on the number of symptoms, how long they last, and how much they get in the way of daily functioning.
- A person suffering from depression may have other problems such as anxiety (or worry), harmful drinking or physical health problems. It is important to treat these problems in addition to treating the depression.
- Depression can be treated either by medication or counselling, or a combination of both.
- HAP is an effective counselling treatment for depression.
1 URL -
Module 2: Healthy Activity Program
Congratulations on completing Module 1 on Understanding Depression! You now have a brief understanding of depression, its symptoms and how to identify it in a patient.
In this module, you will learn about the Healthy Activity Program and its phases.
The Healthy Activity Program (HAP)
- HAP focuses on changing the “action” category of depression symptoms in order to change the other three categories (i.e., body, feelings, and thoughts).
- HAP treats depression by helping patients do activities that are pleasurable and activities that solve problems. We may refer to this as ‘Doing Therapy.’
- As a HAP counsellor, you will help your patients identify specific at-home activities that will help them begin to feel better and solve problems.
- HAP is delivered in a maximum of 8 sessions over three phases.
- HAP focuses on patients with moderate to severe depression as detected by the PHQ 9 questionnaire because patients with mild depression may not need such intensive counselling.
- These forms of counselling are as effective and sometimes preferred to medication in moderate to severe depression.
Phases of HAP Phase Goals Description Manual Section Early Phase (1-2 sessions) Engaging and establishing an effective Counselling Relationship
Helping patients understand HAP
Obtaining a commitment for counselling
Getting started
Understanding problems
Commitment to treatment
Addressing barriers
Counselling Relationship manual Chapter 3 Middle Phase (3-6 sessions) Judging activation targets and encouraging activation
Identifying barriers and how to overcome them
Helping patients solve or cope with life problems
Assessment and activation strategies and problem solving HAP manual Chapter 4: Part 1 & 2
HAP manual Chapter 5
Ending Phase (1 session) Reviewing and strengthening gains the patient has made to prevent relapse Summarising key learnings
Preparing for situations that may trigger depression in the future and generating plans to deal with them
We move through each phase based on whether the goals of the previous phase have been achieved. Some phases may overlap and some patients may remain at one phase for a longer time. The phases are given across six to eight 30-40 minute sessions at weekly (preferably) or intervals of 15 days. A rating scale, called Q-HAP, is used to judge treatment quality during group supervision by an expert supervisor, peer supervisor and peers.
SUMMARY
- HAP is a structured counselling treatment focused on action. It may be referred to as ‘Doing Therapy’
- HAP is delivered in phases, with each phase having its own goals
- The treatment quality is assessed using a quality assessment tool
-
Module 3: Style Of A HAP Counsellor
Congratulations on completing Module 2 on the Healthy Activity Program! You now have a brief idea about the programme and its phases.
In this module, you will revise the style of collaborative counselling.
Key aspects of counselling
Recall the main points learnt during your Counselling Relationship course:
- Maintain session structure
- Focus on action
- Learn collaboratively
- Be non-judgemental
- Acknowledge the patient’s experience
- Be encouraging
- Express warmth and be genuine
-
Module 3: Lesson 1: Maintain Session Structure
Structure shows how a counselling session is different from a friendly chat. It is particularly important while working with patients with depression, who can feel easily overwhelmed and discouraged.
At the start of the session, make an agenda with the patient that includes a list of topics to discuss or tasks to complete. This will provide a guide and make sure that you and the patient focus on what is most important for the session to make progress.
Ensure that the agenda is:
- Collaborative: The session focuses on what matters most to the patient
- Useful: You and the patient have a guide to stay on track with the goals for the session
- Flexible: New topics or tasks can be added by discussing whether to change the original agenda
-
Module 3: Lesson 2: Focus on Action
HAP focuses on action and doing things differently to help the patient feel better. We keep our focus on action and limit the time spent on topics that are not central to the patient taking action to solve problems and feel better.
-
Module 3: Lesson 3: Learn Together Collaboratively
You can work together with your patient by:
- Introducing the patient to each step and making sure they understand the reasons for the steps we suggest
- Having the patient take an active role in the session and by helping set and follow session agenda
- Jointly identifying and planning activities that will be targets for change
- While at the start of counselling it may be necessary for us to take a more active role by directing the session, we always aim to work together by ensuring that the patient understands the reasons for our suggestions. In addition to working with the patient, it may be helpful to also work together with a family member who supports the patient.
-
Module 3: Lesson 4: Be non-judgmental
It can be challenging to work with people with depression when problems arise, such as not completing activities or attending sessions. However, being judgmental of patients - or finding faults - at such times can make counselling harder and make it more difficult to work together with the patient. Practising a non-judgmental style allows us to focus on what happened, rather than on our opinions or reactions and allows collaborative learning.
Often patients have been at the receiving end of judgmental comments from others. Our non-judgmental attitudes can help us build trusting relationships with patients and support the patient in opening up and sharing more with us.
-
Module 3: Lesson 5: Acknowledge the Patient’s Experience
It is important that we recognise the importance of the patients’ experience and show or say that their experience makes sense to us. We may need to accept that when the patient feels depressed, she/he stays away from friends and family, doesn’t complete homework, or fails to attend counselling sessions. It is also important to accept and recognise the importance of the patient’s experience of physical health concerns by explaining the link between physical health and stress, and how HAP will help them feel better.
-
Module 3: Lesson 6: Be Encouraging
We encourage patients every step of the way, looking out for even the smallest signs of progress and improvement. It is our job to help patients set small manageable tasks and encourage even the smallest signs of action and improvement in mood.
-
Module 3: Lesson 7: Express Warmth and be Genuine
Expressing warmth through words and behaviour in ways that are genuine for us can help to establish a positive working relationship with patients. Verbal expressions of care (e.g., “I’m happy to see you today” or “I’m sorry that was so hard”) or non-verbal expressions of warmth (e.g., a smile, body language, eye contact, tone of voice) are simple ways to do this.
SUMMARY
- The Healthy Activity Program counsellor maintains a specific style throughout the counselling treatment.
- Key aspects of this style include setting and following an agenda, keeping the focus of counselling on action, and learning together with the patient.
- It also is important for the counsellor to be non-judgmental, acknowledge the patient’s experience, be encouraging, and express warmth and genuineness.
-
Module 4: Phase 1
Congratulations on completing Module 3 on The Style of A HAP Counsellor! You have now revised the main aspects of collaborative counselling, including maintaining session structure, focusing on action, being non-judgemental, acknowledging the patient’s experience, encouraging progress, expressing warmth and being genuine.
In this module, you will learn about the first phase of the HAP.
-
Module 4: Lesson 1: Overview of Phase 1
Phase 1 is delivered in 1-2 sessions. Watch the video lecture in the activities section below to learn about the structure of Phase 1.
1 URL -
Module 4: Lesson 2: Introducing Yourself
Getting started is a conversation – not a lecture – wherein the patient shares information about his/her life, challenges, goals, and values, and you share information about depression and how to deal with it with HAP by making connections between the patient’s life and experiences.
Prepare yourself before the session, greet the patient and explain about confidentiality. You can begin by asking the patient what brought him/her to the clinic, and after he/she shares their complaint, assure them that the physical problem will be addressed by the doctor. You must also explain that his/her scores show that he/she might have some stress-related emotional difficulties as well and that if he/she allows, you could address these.
-
Module 4: Lesson 3: Establishing Length of the First Session
Most patients will not have planned for a counselling session and some may not be able to stay for the required 30-40 minutes. It is important to check with the patient and together plan how to go forward.
If the patient agrees, we go ahead with a full first session outline by setting an agenda. If the patient says he/she is unable to wait for the entire session, we follow the brief session outline.
-
Module 4: Lesson 4: Setting an Agenda
In the first session, introduce the patient to agenda setting by making a list of items we would like to cover, including:
- Asking about the patient’s problem/s
- Explaining counselling and how it can help them
- Making a plan for future sessions
- Setting the next session date
Always ask the patient if he/she agrees and if there is something to add. Many patients are not used to being active participants, so in the first session you can take the lead in setting the agenda. In later sessions, however, you can first invite the patient to list agenda items to which you then add yours.
Watch the role play video in the activities section below to learn how to set the agenda
1 URL, 1 File -
Module 4: Lesson 5: Getting to Know your Patient
The Healthy Activity model offers a guide to what depression is and how to treat it. You can use this when getting to know the patient and explaining the counselling process to them.
Keep the structure of the session in mind but also allow the patient to share thoughts and feelings without feeling hurried.
-
Module 4: Lesson 6: The First Question
The first question we ask is: “What happened?”
To identify factors that either played a part in starting depression or maintaining it, it helps to identify events or stressors in the patient’s life. However, biological factors are important to acknowledge too.
Often, it is helpful to say, “We think about depression as occurring because of things that happen in your life. Did anything happen when you started feeling down (or stressed)? Or has anything been going on in your life now that makes your life more stressful or harder (or that keeps you feeling down)?” If the patient has difficulty identifying such factors, we can offer possibilities of common factors. We might say, “It’s common for people who are feeling down/ stressed to have struggles with things such as…” A common list of factors might include:
- Severe stress, defined as a difficult event (e.g. death of a loved one, loss of a job, serious accident or injury)
- Long-term stress, defined as problems the patient has been dealing with for a long time (e.g. work-related or relationship problems; lack of safety in one’s neighbourhood or home; long-term financial problems; or having to care for a sick family member)
- Harmful childhood experience (e.g. abuse, neglect or trauma)
-
Module 4: Lesson 7: The Second Question
It is important to understand the patient’s experience of going through difficult situations, what their experience is like now, and what emotions or feelings are experienced in the body. So, you can ask, “When you experience such events (e.g., tension with your husband), how do you feel?”
Common experiences with patients under stress are:
- Sadness and/or irritability
- Low interest or motivation
- Decreased energy - feeling tired and fatigued
- Lowered attention and concentration - inability to study or keep at one task for long
- Thoughts of hopelessness, worthlessness and helplessness
If the patient has difficulty remembering, go back to the items of the PHQ 9 that were scored positive and ask about these experiences. It is very important to explain that these feelings are normal in the face of life’s challenges.
-
Module 4: Lesson 8: The Third Question
You must then identify how the patient responded to the events and feelings that followed. It is helpful to ask: “When you are feeling stressed (sad, tired, etc.), what do you do (or not do)?” It is helpful to explain that is common for people to start or stop doing certain activities that can include:
- Not meeting or talking to friends and family
- Not going to work
- Doing routine activities, e.g. sleeping, eating, hygiene routines, in disorderly ways
- Stopping or reducing physical activity (staying in bed, not exercising, etc.)
- Increasing conflict with people close to them
- Thinking again and again about their problems
If the patient does not easily describe activities, you can ask: “Are there activities you were doing earlier that you have stopped doing since your stress began?”
-
Module 4: Lesson 9: The Fourth Question
Watch the role play video in the activities section below to learn how to describe the HAP model to the patient
Talk about ways in which a patient’s actions, or lack of them, may be keeping them stuck in depression. We can say: “It makes sense that you want to withdraw when you are feeling down, but the problem with this kind of behaviour is that it keeps you stuck in feeling low/down/stressed as you are less engaged in things that make you happy.”
Examples of activities that don’t make you feel good
- Watching TV for hours at a time
- Lying in bed for long periods
- Not attending work
- Not caring for personal appearance and hygiene
HAP counselling works to decrease such activities. Other activities help patients cope or are helpful in their lives, and the HAP counselling works to increase such activities.
Examples of activities that make you feel good
- Speaking to a friend
- Playing with a grandchild
- Spending time in hobbies such as sewing
- Praying or reading religious or motivational books
- Going for a walk
Watch the video lecture in the activities section below to learn about the cycle between behaviour and depression. Watch the role play video in the activities section below to learn about the cycle between behaviour and depression
2 URLs, 1 File -
Module 4: Lesson 10: Suicide Risk Assessment
Calculate suicide risk for all patients. If you find it present, or if the suicide item is positive on the PHQ 9 questionnaire (i.e. item 9), then this becomes the immediate focus of the session. Assessment and management of suicide risk is detailed in the PREMIUM Counselling Relationship Manual.
-
Module 4: Lesson 11: Specifics of Counselling
It is important to give the new patient some information about HAP that includes:
- Our training and by whom you are supervised
- How long the counselling takes – the number of sessions and over how much time
- Where the sessions will be conducted – at home, in the clinic or over the telephone
- How you can be contacted outside the sessions, and in what situations
Ask the patient if they have any questions about the treatment and respond to them as best as you can.
You can provide encouragement by asking how life would be different if their stress or tension was addressed and providing hope that through the process of counselling, they can be treated.
FAQs about the specifics of counselling FAQs Answers Are medicines not enough? Counselling is known to increase the chances of getting well. The benefits can last even after the sessions are completed. You can continue to receive medicines from the doctor for your other health problems during the counselling. What if I cannot come to the clinic to see you? We can have sessions at your home if this is ok with you. We can also speak on the phone if you are unable to come to the clinic. Let me know which option you prefer. Can you speak to my husband/wife/sister/mother to solve my problem with them? I will be very happy to meet your relative so he/she can understand the nature of your problem and what they may be able to do to help. Please ask them to read this handout and bring them with you when we meet next. It will be very useful to have them involved in your treatment. Can this counselling really help me? I am already doing so many activities but I still feel stressed We will be working together to examine these activities and see how we can use them to help you feel better. We will also discuss ways to deal with the problems in your life. This counselling has helped many people with problems like yours. Let us try it and see the results -
Module 4: Lesson 12: Involving a Significant Other (SO)

People with depression may not talk about their experiences openly and may wonder why they cannot make themselves feel better. An important part of counselling involves helping family members understand what depression is and ways to treat it.
Here is a review from the Counselling Relationship course on ways to involve the significant other (SO), such as a close family member or friend the patient trusts:
- Ask the patient if they would like the SO (who has come with them to the clinic) to stay for the entire session. Some may only want the SO to join in when you explain HAP and the details of counselling.
- Discuss with the patient the possible benefits of involving the SO in counselling.
- While it is useful to involve the SO, it is not essential.
- If the SO attends the session, ask the person if he/she wants to provide more information on the patient’s problems and if he/she has questions.
- Encourage the SO to read the handout and return with any questions he/she may have.
-
Module 4: Lesson 13: Eliciting Commitment
To get the patient to commit to the treatment, we need to give him/her time to talk about their understanding, clear their doubts, and go over parts they may not have understood.
-
Module 4: Lesson 14: Addressing Barriers
It is important to explore problems that may interfere with the patient's participation in the treatment. In the case of a patient refusing treatment, we might dig further into their reasoning.
Barriers Solutions Patient level Cannot attend counselling sessions due to practical barriers such as
- Transport cost
- Lack of time
- Care-giving responsibilities
- Age
Home visits can be the first option, followed by telephone counselling, with flexibility in scheduling sessions.
Discuss with the patient how to get the help of those who can take over their care-giving responsibilities in their absenceThe SO, usually the patient’s husband, does not allow counselling Invite the SO to engage in the counselling process if he/she has come with the patient to the clinic. If not, encourage the patient to share the handout with the SO and then invite him/her for participation No time to wait for the first session Time of the session shortened with a focus on engagement and addressing problems to follow-up Significant social stressors such as financial problems and does not see how ‘talking’ will help Explain that you can help address social stressors, and do so as soon as possible through referral for appropriate services or problem-solving Preoccupied about physical health and blames problems only on physical illness Physical illness beliefs to be taken care of. Explain the mind-body link. Stress on the role of physical symptoms in depression States preference for medication rather than counselling Explain that counselling is an option in addition to medical treatment, not instead of, and can further improve the chances of long-term recovery Uncommunicative and doesn’t open up about problems Spend greater amount of time in engaging and explaining how treatment will help.
Assure the patient that all information will be confidential.
Speak to the patient alone if he/she has come with the SOSuffering from personal crisis Allow time for the patient to show sadness or emotional pain. Follow the steps in dealing with a personal crisis (as learnt in the CR course) and postpone the other tasks of session 1 to later sessions PHC level Counsellor not seen as part of PHC team Request the doctor and other staff to encourage the patient to receive counselling Counsellor level Failure to engage patient The first session is a conversation. It is important to allow time for listening to the patient’s experience. It is also important to share your knowledge so that the patient has correct information about counselling.
Provide patient material.
Actively involve the SO and get their help in making sure the patient attends counselling sessions -
Module 4: Lesson 15: Addressing the Patient's Chief Concerns
In order to effectively engage the patient in counselling, address her/his main concerns. These may include social problems for which there are existing welfare schemes in which we can discuss how they can access these, or sleep problems that we can provide simple tips for. If there are problems that require urgent attention, begin the steps of problem solving in this session. Otherwise, reassure the patient that you will help them address this problem in future sessions.
-
Module 4: Lesson 16: Planning Homework
Encourage patients to do work in between sessions.
First, explain the homework: At the end of the first session the patient is given the booklet and the handout with information for the significant other.
If the patient is unable to read, ask if they can request someone in their family to read it to them.
Then ask for problems in performing the homework and help solve them.
At the end, remind them that in the next session you can both discuss what the patient has understood about counselling.
-
Module 4: Lesson 17: Summarising
Summarising refers to giving a short but complete description of the session that includes the key points that were discussed and the homework for the coming week. It allows the patient to briefly describe the information so that you can understand how successfully you communicated and whether you need to correct any doubts/misunderstandings.
After the patient says what they have learned, repeat their ideas and, if necessary, add anything they have left out.
-
Module 4: Lesson 18: Setting the Next Session Date
Set the time and place of the next session together with the patient, aiming to arrange it after seven days at the patient’s home. Be flexible depending on what is convenient for the patient. Arrange telephone sessions in between the home visits and clinic visits even if it is short. Note all contacts and enter the next session date in the phone diary with a reminder to call the patient before the upcoming session.
If the patient is not keen on a home visit, encourage them to come to the PHC. Ask if they are meant to come to the clinic for a follow up, fix an appointment to suit this timing. If neither is possible, confirm that you will have a telephone session.
After the patient leaves, complete the clinical record form and the daily register.
-
Module 5: Phase 2
Congratulations on completing Module 4 on Phase 1 of the Healthy Activity Program! You now have an overview of the first phase of the HAP treatment. This includes introducing yourself and agreeing on the length of the session, setting an agenda and getting to know the patient. It also involves asking important questions about the patient’s problem, assessing suicide risk, talking about counselling, involving a significant other, addressing problems and the patient’s chief concerns, planning homework and summarising.
In this module, you will learn about the second phase of the HAP treatment.
-
Module 5: Lesson 1: Overview
Phase 2 is delivered in 2-6 sessions over two parts – Learning Together, and Getting Active and Solving Problems.
The goal of learning together is to identify activation targets. The phase includes checking progress, setting an agenda, going over homework, learning together, encouraging activation, involving a significant other in learning together, planning homework (including addressing barriers), summarising, setting the next session date and keeping records.
During phase 2, select treatment targets by defining the patient’s goals and helping him/her achieve them.
-
Module 5: Lesson 2: Learning Together
- Review progress
First, review the patient’s progress by comparing the current PHQ-9 score with the one from the previous visit and provide feedback to the patient. Remember to assess and manage suicide risk as a priority based on the patient’s current score.

- Set the agenda
Then, explain the importance of setting an agenda and mention that the patient ought to actively participate with you in the HAP treatment process. Give them time to add suggestions to the agenda or ask questions. Go over the problems discussed in session 1 and ask if the patient needs to talk about any of them.
Go over new problems and ask if the patient would like to discuss any of them. List agenda items including discussing homework, recording the patient’s activities and how he/she feels when doing them, planning to identify at least one activity that can help them feel better and scheduling it until the next session, setting the next session date, and asking the patient if they agree with the list and have anything else to add.
- Review homework
Ask directly if they did the homework or have any questions about what they read. You can ask them to describe what they understood about the treatment and fill in the gaps or correct any misunderstanding. If the patient did not do the homework, ask directly but non-judgementally what happened.
This helps understand what obstacles the patient is facing and leads towards helping them overcome these obstacles. It is common for patients to not complete the homework. You can complete the assignment during the session so the responsibility of completion is shared and the patient feels supported.
1 URL, 1 File -
5.2a Collaborative Learning and the HAP Model
The counsellor and patient know which activities will help the patient feel better, solve problems and achieve goals by learning together to identify links between the patient’s activity and mood. Go over the activities the patient is involved in and how they affect his/her mood. You can then plan how to increase the activities that make them feel better and decrease the ones that don’t through problem solving. Use terms like ‘things that make you happy’ or ‘things that make you sad’ to help them understand better.
You can identify these activities through:
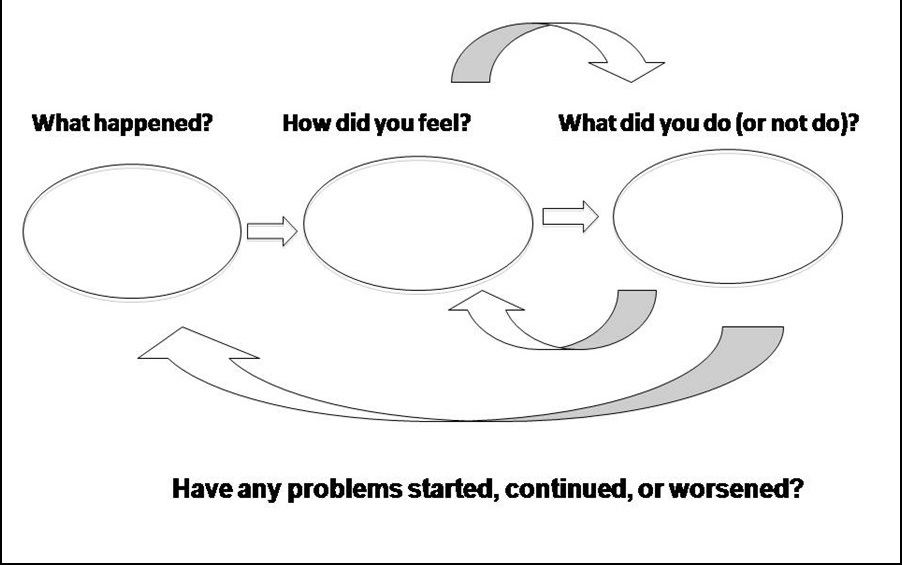
- The HAP model: When patients come to sessions with concerns about the period since the previous session (such as times when they felt down), ask about the situations, specifically about the parts of the Healthy Activity Program: ‘What happened?’, ‘How did you feel?’, ‘What did you do or not do?’, ‘What connections were present between what you did and how you felt?’
- Activity Calendar: Record the patient’s activities and moods at the time of doing the activities. Explain why filling the calendar is important by reminding them about the HAP model and how activities can affect mood and stress. Go through the patient’s day with him/her and how they felt at each point. If the patient uses words in physical terms such as ‘tension’ or 'feeling well/unwell', use the same words to explain the mood rating. Identify any links between activity and mood with the patient.
MOOD LADDER
 Ask the patient to rate his/her mood along the steps of the calendar, with the lowest step as the worst he/she has felt and the top step the best.
Ask the patient to rate his/her mood along the steps of the calendar, with the lowest step as the worst he/she has felt and the top step the best.- Good/Bad: For those who do not report strength of mood in detail, ask them to choose whether they feel ‘happy or sad’ or ‘good or bad’.
- Emoticons: For those who cannot read or write, use icons to identify how they are feeling.
- Tick and cross: Use a tick mark to show positive mood and a cross to show a negative mood.
-
5.2b Involving a Significant Other
- For the elderly or those who cannot read/write, if the SO has been involved in the treatment process, discuss the option of having the SO write the activity calendar for the patient.
- The SO can remind the patient at regular times to fill in the activity calendar and encourage them to do the planned activity that helps them feel better.
-
5.2c Planning Homework and Overcoming Barriers
Based on the activity calendar, identify one activity that helps the patient feel better and together discuss a specific plan to do this activity at home. Encourage the patient to follow it at scheduled times until the next session and fill in the calendar. Explain that noting the activity and rating the mood will help them see the relationship between doing activities and feeling better.
Prepare the patient for possible barriers by thinking of solutions with them.
Barriers Challenges Difficulty in remembering to do the activity or fill the chart Link the activity and completing the chart to another routine activity such as meal time.
Use reminders such as stickers in prominent places.
Involve the SO to remind the patient.No time to do the activity and/or fill the chart Help the patient identify a possible time when he/she may be more likely to do the activity and/or fill the chart.
Ask the patient to fill the chart only once in the dayPatient cannot read/write Help the patient identify an SO to fill the chart.
Use a chart with pictures.Does not understand the reason to do the activity and/or fill the chart Revisit the Healthy Activity Program, the link between activities and mood, and the idea of activities that make them feel better and those that don’t Finally, summarise the discussions and activities of the session, set the date for the next session and complete the clinical form after the patient leaves.
-
Module 5: Lesson 3: Getting Active and Solving Problems
The goals in these sessions are to strengthen the understanding of the HAP and apply it to daily life, encourage activation, identify barriers to activation and learn how to overcome them, and help patients solve or cope with life problems. Like before, these sessions include keeping a check on progress, setting an agenda, going through homework, getting active, solving problems, involving the SO, dealing with problems, planning homework, summarising, setting the next session date and completing documents.
In these sessions, patients will learn the skills they need to get active and address problems through homework.
- Review progress as before, along with suicide assessment
- Set an agenda
Ask the patient about the homework that was to be done, go over the activity chart together and select activities that can help the patient. Plan to perform these activities and discuss ways to deal with problems the patient is facing.
- Review homework
Ask the patient whether he/she has filled the activity plan and the experience he/she has had. Find out about links between the activities and the patient’s mood, any patterns that you notice, how well routine activities support the patient’s mood. In later sessions in the same phase, you can ask about specific activities they were meant to do. Encourage progress the patient has made on the action plan, and go over what was done or not done in detail.
1 URL, 1 File -
Module 5: Lesson 4: Solutions to Overcome Barriers and Complete the Activity Plan
Barriers/Challenges Solutions Does not fill the activity plan or says he/she cannot fill the plan Explore the reasons why.
Explain in detail why he/she should fill the plan.
Try filling the plan in the session.Writes an activity, such as ‘at work’, that is not specific for a large duration Ask detailed questions – ‘what he/she was doing’, ‘with whom’, ‘for how long’ – to define the behaviour.
Tell the patient you want to learn enough about their activities that you could repeat the actions based on the description, such as making ‘rice and fish curry and chicken for the children’s treat’, instead of simply ‘making dinner’.Reports an activity that might be causing problems but you are not certain how important it is for the patient’s mood Ask more about how often they do the activity and for how long, and whether there has been an increase or decrease. Reports feeling worse during an activity but you do not understand what led to the worsened mood Ask more questions to understand the situation the activity occured in. For example, through further questioning, you can learn that a woman may say she has more anxiety whenever she enters the kitchen because her mother-in-law made a negative remark that caused her to give up and go to bed. Did not carry out the activities as planned despite attempting to do so Go over the activity plan and cut back on the number and/or frequency of activities.
Change the activity to something that is easier. -
Module 5: Lesson 5: Getting Active
The target activity is identified through a joint effort of assessment. It is helpful to begin with activities that make the patient feel better and that the patient is more likely to do. Even though the first actions do not address the main problems, they help the patient feel more positive and prepared to tackle bigger problems.
Watch the role play video in the activities section below to learn how to get a patient do activities
1 URL, 1 File -
Module 5: Lesson 6: Breaking Down the Activity
Focus on helping patients break down more complex behaviours. For example, to spend more time with the family, the patient could return home from work an hour earlier, sit and read a newspaper in the same room where the children are playing, watch the children at play and participate in play with them.
-
Module 5: Lesson 8: Solutions to Overcome Difficulties in Doing an Activity
Barriers/Challenges Solutions No time to do the activity Help the patient plan a particular time and day for the activity.
Help the patient think of how they can reduce other tasks and make time for the activityThe patient says they may forget to fill the chart/do the activity Keep the plan in a place where it is easily seen at home.
Involve the SO in reminding the patient.
Set an alarm/reminder on a clock/telephone.Lacks confidence about doing the activity, says they may feel too low/stressed Highlight how the activity will help the patient feel better, go over the Healthy Activity Program briefly.
Discuss who may be able to help him/her with the activity.
Involve the SO in encouraging the patient to do the activity.
Go over the activity and break it down into smaller steps, and encourage the patient to start with one step at a time.1 URL, 1 File -
Module 5: Lesson 9: Solving Problems
Patients with depression often face problems to do with finance, relationships, health or difficulty in doing routine activities. Their experience of these problems is often closely linked to their symptoms, so problem solving is an important form of activation for many patients.
Watch the video lecture in the activities section below to learn about problem solving.
1 URL -
Module 5: Lesson 11: Possible Solutions to Common Problems
Problem Possible Solutions Family member has a drinking problem - Person concerned can be encouraged to seek treatment by asking the patient to share the hazardous drinking brochure
- People close to the family member can encourage and support him/her to stop drinking
Physically abusive spouse - Seek the help of someone who may be able to speak to the spouse
- Discuss safety measures
- Referral to support agencies
Patient does not have a job - Explore options of job opportunities such as ads for vacancies
- Ask friends and family to explore their network
- Share information about government employment schemes
Illness in the family - Encourage the family to seek the right treatment
- Follow medical advice
- Refer the person to a specialist/agency/hospital
- Care for the person’s needs suitably
- Seek support for oneself to deal with the burden of care
Relationship difficulties - Identify ways of communicating better
- Ask the person close to the patient to come for a session
- Involve a third person who can help the patient
Financial difficulties - Look for better job opportunities
- Refer to government schemes such as pension schemes
- Explore ways of saving
- Seek help from friends/family
A person in the family with special needs - Seek professional help to support the person
- Gather information and enhance skills to care for the person
- Seek support for oneself to deal with the burden of care
- Refer to an agency
Difficulty in coping with work stress - Learn useful ways to cope with stress, such as taking short breaks
- Time management
- Improve skills that will help with work performance
- Seek support from seniors/co-workers
Stress and loneliness caused by living away from home and family - Maintain regular communication with family
- Create a support network of friends
- Join community activities
Elderly patients with no family support - Explore possibility of building a support network
- Provide information about government schemes
- Refer to agency
-
Module 5: Lesson 12: Involve SO in Activation and Problem Solving
The SO can help:
- Identify activities that make the patient feel better and those that do not, in addition to what the patient may have reported
- Identify a problem and generate solutions when attempting to solve problems in the patient’s life
- Support the patient in doing the activities
- Help the patient record the activities in the chart
- Support the patient in coming for sessions and come along with them if required
-
Module 5: Lesson 13: Planning Homework
The homework will focus on helping the patient get active with doing activities that make them feel good and/or doing activities related to solving problems. Develop specific homework together with the patient based on an assessment of the links between activities and mood of the patient.
List out the agreed activities in the chart in the patient booklet, against which the patient puts a tick when it has been performed during the week. They also record their mood. Fill in the chart at the next session if the patient has not filled it at home.
Measure the degree of activation by listing out the activities and asking the patient to share feedback on what extent they were performed on a 4-point scale given in the clinical record form. Remember to plan for problems or barriers and help the patient understand that he/she may not complete all of the activity due to these.
Finally, summarise, set the next session date and complete the documentation once the patient leaves.
-
Module 6: Phase 3
Congratulations on completing Module 5 on Phase 2 of the Healthy Activity Program! You now have an overview of the second phase of the HAP treatment. This includes teaching the patient how to get active and solve problems, dealing with problems in completing the activity plan, breaking down activities, overcoming difficulties in doing activities, the importance of problem solving, solutions to common problems, involving a significant other in activation and problem solving, and planning homework.
In this module, you will learn about the third phase of the HAP treatment.
-
Module 6: Lesson 2: Introduction to Phase 3
Ending well aims to identify possible triggers that may increase the risk of having another depressive episode, and address these by going over what helped during counselling and how to continue these actions in future.
1 URL -
Module 6: Lesson 4: Set an Agenda
Ask the patient what he/she would like to discuss. Make a list to be covered during the session, including asking about homework, going over skills the patient has learned and activities that affect mood positively, and summarising steps to help support the patient in staying well over time. As always, ask the patient if he/she agrees with the list and whether he/she would like to add anything to it.
-
Module 6: Lesson 5: Review Homework
Ask the patient about the homework, including what they learnt from doing the activities planned, the barriers they faced, etc. You can also ask about particular activities, for example things they noticed when doing steps to reduce fights with their husband/wife.
-
Module 6: Lesson 6: Review Skills Learnt
- Ask the patient to explain in their own words what they learnt from the previous sessions.
- Clarify information that is not clear.
- Highlight steps the patient used to overcome depression in the past.
- Emphasise the patient’s role in getting better.
- Motivate patients to use strategies in other life situations, such as using actions to solve fights with a husband/wife when dealing with seniors at the workplace or other family members.
-
Module 6: Lesson 7: Summarise for Prolonged Wellness
Fill in the End of Treatment form with the patient by:
- Listing activities that the patient needs to maintain or increase
- Identifying situations that might make it harder for the patient to keep doing the activities that make them feel better. Go over activities that the patient found useful during counselling
- Asking the patient what situations might increase the risk of developing tension in the future. Knowing stressful situations in advance can help them take action to protect themselves
- Asking the patient what activities they may start doing again and alerting them to the early warning signs of depression
- Discussing what can help during difficult situations
-
Module 6: Lesson 8: Involving a Significant Other
The SO can help:
- Encourage the patient to continue engaging in activities that help them feel better
- Identify stressors that may cause tension and aid the patient in finding solutions
-
Module 6: Lesson 9: Summarise Session
As in previous sessions, help the patient summarise what was done in this session. Then, repeat what he/she has learnt and add things he/she might have left out.
At the end, thank them for their participation, ask about any remaining questions and remind them of the contact details in case they need additional help.
- If a patient remains unwell at the end of eight sessions, refer him/her to an independent psychiatrist
- If a patient who has dropped out returns, offer counselling and continue from the last session
- If a patient who has been discharged returns seeking help, encourage him/her to consult the PHC doctor or refer him/her to the psychiatrist. No further session is offered.
Finally, complete the clinical record form and end of treatment evaluation form.
-
Module 7: Strategies For Thinking Too Much
Congratulations on completing Module 6 on Phase 3 of the Healthy Activity Program! You now have an overview of the third phase of the HAP treatment. This includes going through homework and skills the patient has learnt, summarising steps to help the patient stay well over time, involving a significant other in staying well and ending well.
In this module, you will learn about the problem of thinking too much and how to help the patient deal with it.
-
Module 7: Lesson 1: Understanding the Problem
Patients often think about themselves and how they feel, the condition they are in, and the reasons for their struggles. They describe this experience – repeating thoughts about these topics in their mind – as ‘thinking too much’. This problem can make it hard for some patients to do activities, such as taking a walk in the park.
1 URL -
Module 7: Lesson 3: Reviewing Strategies
Watch the video lecture in the activities section below to learn how to go over your strategies when dealing with a patient who thinks too much
Watch the role play video in the activities section below that shows how to help a patient who thinks too much
2 URLs, 1 File -
Module 8: Strategies For Feeling Anxious & Tense
Congratulations on completing Module 7 on Thinking Too Much! You now understand the problem of thinking too much and how to help the patient who does so.
In this module, you will learn about the problem of feeling anxious and tense.
-
Module 8: Lesson 1: Overview
Remember that some types of anxiety require additional help. If the patient’s anxiety is severe and constant, or occurs in brief sudden episodes, refer him/her to a specialist.
1 URL -
Module 8: Lesson 3: Teaching Breathing Exercises

Guide the patient through the steps of the breathing exercise during the session. Then let the patient continue in silence for about 3-5 minutes. Finally, ask the patient what he/she experienced in order to identify any questions, problems or confusion. If necessary, guide the patient through the exercise again.
Once the patient has learnt the exercise, ask him/her to do it at home regularly. Discuss the length, frequency, place and possible difficulties in doing the exercise.
- Posture
Any position the patient finds comfortable is fine. The exercise is usually practised with the eyes shut, but if the patient is more comfortable with the opposite, he/she may leave his/her eyes open.
- Breathing
After 10 seconds, the patient should focus on the rhythm of his/her slow, regular, steady breathing. Rhythms can be suggested at three counts while breathing in, three counts for breathing out, and a pause for three counts until the process is repeated. The patient could say ‘relax’ or something similar in the local language in his/her mind each time he/she breathes out. Patients who are religious could use a word important to their faith.
Continue the exercise for 10 minutes until the anxiety has reduced. If the patient complains of any physical discomfort during the exercise, slow down the rhythm to one that is more comfortable.
Refer the patient to information about relaxation in the patient booklet, which they can read at home or get a relative to read for them.
-
Module 8: Lesson 4:Review Strategies
Watch the video lecture in the activities section below to learn the main points of reviewing strategies to deal with the problem of feeling anxious and tense.
Watch the role play video in the activities section below on assessing how the patient deals with his/her anxiety and how to help him/her
1 URL -
Module 9: Problems With Close Friends/Family
Congratulations on completing Module 8 on the Strategies For Feeling Anxious And Tense! You now understand the problem of feeling anxious and tense and how to help the patient deal with it through relaxation techniques.
In this module, you will learn how people close to the patient might affect them and how to deal with problems that might arise.
-
Module 10: Dealing With Sleep Difficulties
Congratulations on completing Module 9 on the Problems With Close Family/Friends! You now know how to teach the patient to manage problems with people close to them through effective communication.
In this module, you will learn how to find the causes for difficulties with sleep and the techniques to help the patient deal with them.
-
Module 11: Dealing With Tobacco Use
Congratulations on completing Module 10 on Dealing with Sleep Difficulties! You now know the techniques to help patients who have trouble sleeping.
In this module, you will learn about the relationship between tobacco use and depression and how to help the patient deal with it
-
Module 12: Medication
Congratulations on completing Module 11 on Dealing With Tobacco Use! You now know the relationship between tobacco use and depression and how to help the patient deal with it.
In this module, you will learn how medicines work in helping to deal with depression, when they are used and what your role is with a patient who has been prescribed medication.
-
Module 12: Lesson 1: Medicines in Depression
The group of medicines used to treat depression is called ‘antidepressants’, which are used as an alternative or in addition to counselling to treat people with severe depression.
Evidence suggests that antidepressants work by changing the brain’s chemical profile. This process takes a few days to two weeks, causing a ‘lag period’ before they begin to show results. The chemicals changed by the antidepressants are also present in other parts of the body and also get affected. This may cause side effects before the patient starts feeling better. These points – the lag period and side effects – must be communicated to the patient to help support antidepressant treatment.
-
Module 12: Lesson 2: Usage
Knowing the names of the antidepressants will help you recognize them when the doctor prescribes them to the patient you are counseling.
They can be started along with counseling when the patient is first found to have depression, or added to ongoing counseling if the patient does not improve after two consecutive sessions or worsens despite counseling. Some patients may refuse counselling or may be unable to participate. In such cases, they can be offered antidepressants as an alternative form of treatment.
-
Module 12: Lesson 3: Counsellor's Role

Explain the following points to the patient:
- Antidepressants are widely used and have benefitted many by helping to reduce symptoms and improve overall health
- They are not addictive
- They may produce side effects, but these are not common, mild and short-term
- They may take up to two weeks to begin showing positive effects
- It is important to take them regularly for maximum benefit
- It is important to take them as prescribed by the doctor, even if one feels an improvement. Stopping the medicines before the suggested time frame can cause the problems to return
- Taking them regularly is an important activation target. Explore possible barriers and solutions
- Report any unusual or severe side effects to the supervisor, who can discuss them with the doctor. Always encourage the patient to talk to his/her doctor about any questions about the medication or side effects
Refer the patient to the patient booklet to help them understand better.
1 Quiz -
Course and Self Evaluation & Certificate
 In this section, you can provide feedback about this course to help us make NextGenU.org better. Once evaluations are completed, you will be able to download your certificate of completion.
In this section, you can provide feedback about this course to help us make NextGenU.org better. Once evaluations are completed, you will be able to download your certificate of completion.

