Resources Lesson 1: Maternal Mortality - Epidemiology and Causes
How the epidemiology of maternal mortality (including the role of cultural, social, and behavioural factors) can help understand its causation.
We can get a great deal of information from routine data, given the limitations we discussed in Topic 1. Maybe we can start with an exploration of the geographical and social inequalities in distribution. WHO has an interactive graph to show the between-country variation Maternal Mortality. A 2019 report Maternal deaths decline slowly with vast inequalities worldwide shows that "For women, this means that the global lifetime risk of maternal mortality – the risk that a 15-year old girl will die eventually from a maternal cause – was approximately 1 in 190 for 2017, nearly half of the level of risk in 2000. Not surprisingly, maternal deaths in the world’s least developed countries are high, estimated at 415 maternal deaths per 100 000 live births with the lifetime risk as high as 1 in 37 for a 15-year old girl in sub-Saharan Africa. In comparison, the same girl living in Australia or New Zealand would have a risk of just 1 in 7800." The within-country variation in maternal mortality is also considerable, as described in this paper Levels and determinants of maternal mortality in northern and southern Nigeria.
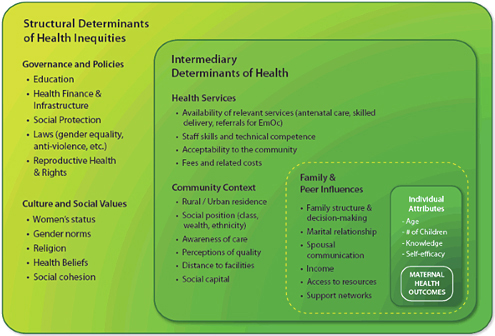
There are also social and behavioural causes, as described in this page from WHO Social determinants approach to maternal deaths. The picture below comes from this site:
Further exploration of the social determinants, as in this file from the UNFPA 'Rich mother, poor mother' may give us some clues about the causes.
More on causes comes from this paper Global causes of maternal death: a WHO systematic analysis, which found: "haemorrhage, hypertensive disorders, and sepsis were responsible for more than half of maternal deaths worldwide. More than a quarter of deaths were attributable to indirect causes. These analyses should inform the prioritisation of health policies, programmes, and funding to reduce maternal deaths at regional and global levels" and again that "Further efforts are needed to improve the availability and quality of data related to maternal mortality."
A major cohort study Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa: a multi-country prospective cohort study, in many ways more powerful than using routine statistics since the cohort was followed using verbal autopsies, ".. identified 278 186 pregnancies and 263 563 births across the study sites, with outcomes ascertained for 269 630 (96·9%) pregnancies, including 8761 (3·2%) that ended in miscarriage or abortion. Maternal mortality ratios in sub-Saharan Africa (351 per 100 000 livebirths, 95% CI 168–732) were similar to those in south Asia (336 per 100 000 livebirths, 247–458), with far greater variability within sites in sub-Saharan Africa. Stillbirth and neonatal mortality rates were approximately two times higher in sites in south Asia than in sub-Saharan Africa (stillbirths: 35·1 per 1000 births, 95% CI 28·5–43·1 vs 17·1 per 1000 births, 12·5–25·8; neonatal mortality: 43·0 per 1000 livebirths, 39·0–47·3 vs 20·1 per 1000 livebirths, 14·6–27·6). 40–45% of pregnancy-related deaths, stillbirths, and neonatal deaths occurred during labour, delivery, and the 24 h postpartum period in both regions. Obstetric haemorrhage, non-obstetric complications, hypertensive disorders of pregnancy, and pregnancy-related infections accounted for more than three-quarters of maternal deaths and stillbirths. The most common causes of neonatal deaths were perinatal asphyxia (40%, 95% CI 39–42, in south Asia; 34%, 32–36, in sub-Saharan Africa) and severe neonatal infections (35%, 34–36, in south Asia; 37%, 34–39 in sub-Saharan Africa), followed by complications of preterm birth (19%, 18–20, in south Asia; 24%, 22–26 in sub-Saharan Africa)."
Other leading causes of maternal mortality are related to mental health issues that lead to suicide, drug overdose, and drug use-related complications.
Suicide during pregnancy is frequently related to intimate partner violence and chronic mental health issues. The frequency of pregnancy-associated death due to drug overdose varies with geographical location. From 2005 to 2014, drug-related maternal mortality was approximately 26% in Utah, and in Maryland, 38% of maternal deaths were associated with drug use in 2019; this may be due to the significant number of pregnant women who have one or more psychiatric diagnoses related to other factors such as intimate partner violence. Thus, the issue of maternal mortality and drug use must be addressed from multiple approaches in an individualized and comprehensive manner, involving treatment without prejudice. Read the content under the headings "Abstract," "Pregnancy-Associated Suicide," "Drug Overdose During Pregnancy and Pregnancy-Associated Death," "Risk factors of pregnancy-associated death by drug overdose," and "Prevention of pregnancy-associated death by drug overdose."
The picture of a combination of geographical, social and health care factors that underlie the causes of maternal mortality is becoming clear. Take a look also at this paper from Ethiopia Trends and causes of maternal mortality in Ethiopia during 1990–2013: findings from the Global Burden of Diseases study 2013 for an example of country-specific data on causes. Let's also get back to the WHO fact sheet Maternal mortality as a review. We will next spend some time on the health system issues.
Broadening the scope:
Here is another paper from the 2016 Lancet series on maternal health: Diversity and divergence: the dynamic burden of poor maternal health. Causes of poor maternal health are increasingly diverse and locally determined, as described in this paper, and it describes well the need to include morbidity as the hidden part of the iceberg, of which the visible tip is formed by maternal mortality. Only focusing on mortality will not easily solve the matter, if the underlying maternal morbidities are not co-addressed. It also show clearly how the pattern of causes of mortality and its distribution within and between populations have changed over time.
This paper: How are the domains of women's inclusion, justice, and security associated with maternal and infant mortality across countries? Insights from the Women, Peace, and Security Index is an example of how matters not traditionally associated with health are of considerable importance in the topic of maternal mortality (gender inequality: women’s inclusion, justice and security).
Also this paper: Abortion laws reform may reduce maternal mortality: an ecological study in 162 countries shows how abortion law influences maternal mortality.
How problems of your health services system may cause inadequate perfomeance of health service and contribute to the problem of maternal mortality and morbidity.
There are three papers from the 2016 Lancet series which provide some examples of how health service systems, after all just another social determinant of health, are related to causation: limiting access to family planning for young or unmarried women, excessive use of caesarean section, problems in abortion care, etc. These first three papers are only available as abstracts, but each refers and provides links to a number of other papers in the series:
The scale, scope, coverage, and capability of childbirth care : "The necessity of ascertaining actual facility capability and providers' skills is highlighted, as is the paucity of information on maternity waiting homes and transport as mechanisms to link women to care. Furthermore, we stress the importance of assessment of routine provision of care (not just emergency care), and contextualise this importance within geographic circumstances (eg, in sparsely-populated regions vs dense urban areas).....Conceptualisation, systematic measurement, and effective tackling of coverage and configuration challenges to implement high quality, respectful maternal health-care services are key to ensure that every woman can give birth without risk to her life, or that of her baby."
Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis finds that "A quarter of all women who died in LMICs (72 studies, 27 651 deaths) had undergone a caesarean section (23·8%, 95% CI 21·0–26·7; τ2=0·62)...Maternal deaths and perinatal deaths following caesarean sections are disproportionately high in LMICs. The timing and urgency of caesarean section pose major risks."
Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide finds "On the continuum of maternal health care, two extreme situations exist: too little, too late (TLTL) and too much, too soon (TMTS). TLTL describes care with inadequate resources, below evidence-based standards, or care withheld or unavailable until too late to help. TLTL is an underlying problem associated with high maternal mortality and morbidity. TMTS describes the routine over-medicalisation of normal pregnancy and birth. TMTS includes unnecessary use of non-evidence-based interventions, as well as use of interventions that can be life saving when used appropriately, but harmful when applied routinely or overused.....Health-care providers and health systems need to ensure that all women receive high-quality, evidence-based, equitable and respectful care. The right amount of care needs to be offered at the right time, and delivered in a manner that respects, protects, and promotes human rights."
Unsafe abortion is also a health systems issue, as shown in this paper: Unsafe abortion and abortion-related death among 1.8 million women in India: "Despite abortion being legal, the high estimated prevalence of unsafe abortion demonstrates a major public health problem in India. Socioeconomic vulnerability and inadequate access to healthcare services combine to leave large numbers of women at risk of unsafe abortion and abortion-related death"
Contraceptive services. Bias in Contraceptive Provision to Young Women in South West Nigeria (the link takes you to a download service for the paper) - the paper concludes: "Provider bias in the provision of contraceptives to adolescent and young adult women in South West Nigeria may affect quality of care and method choice. Interventions to reduce provider bias should go beyond technical training to address the underlying sociocultural beliefs that lead providers to impose restrictions that are not based on evidence."
Variation in quality of care. The paper Not all inequalities are equal: differences in coverage across the continuum of reproductive health services shows "that dominant inequalities in contraceptive coverage are varied, and include large disparities and impact by age group, compared with maternal health services, where inequalities are largest by economic status and urban–rural residence. Using multiple measures of inequality (relative, absolute and population impact) not only helps to show if there are consistent patterns in inequalities but also whether few or many different approaches are needed to reduce these inequalities and where resources could be prioritised to reach the largest number of people in need."
